Ajmaline Study
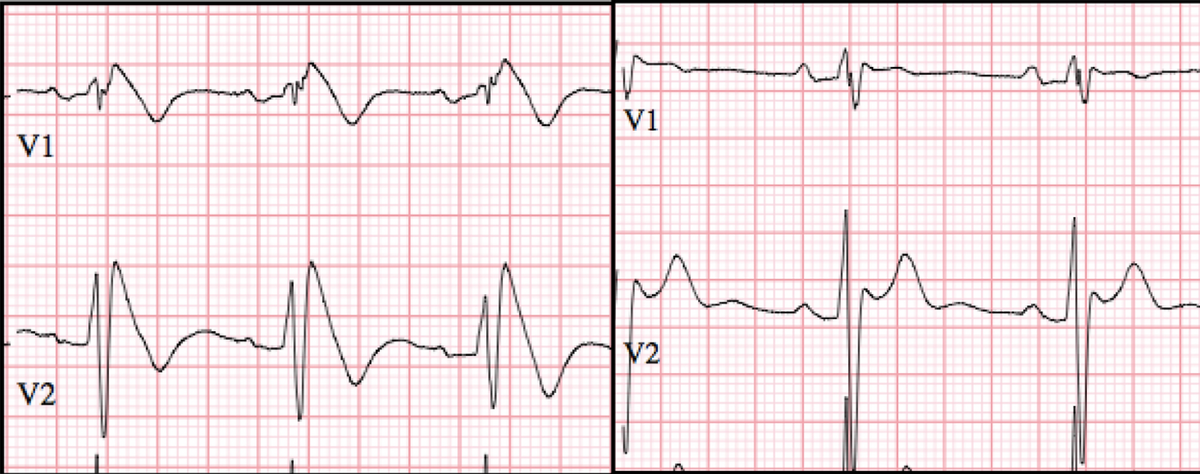
The Ajmaline Study is a test performed in hospital to bring out the ECG changes of Brugada Syndrome
Brugada Syndrome is an electrical disorder of the heart which may cause syncope (fainting) and cardiac arrest. However, the majority of patients with Brugada Syndrome have no symptoms.
Reason for Performing
Brugada Syndrome is diagnosed on a 12 lead ECG, usually in the context of typical symptoms or a family history of the disorder. Sometimes, the ECG changes of Brugada are discovered incidentally when an ECG is performed for another reason e.g. chest pain.
However, it is now known that the ECG changes of Brugada Syndrome may come and go, being present one day and not another. Therefore, when typical symptoms occur in an individual or their relative it is difficult to know if Brugada Syndrome is the cause.
An Ajmaline Study may ‘bring out’ the typical ECG changes of Brugada Syndrome which would otherwise remain concealed.
How Is it Performed?
After admission to hospital, in a fasted state, an ECG is performed. If Brugada is present on this ECG then the Ajmaline test is not performed. But if it is not, then an IV line will be placed in a vein in your arm. Under strict cardiac monitoring, Ajmaline is injected (1mg/kg up to 100mg) over 5-10 minutes. An ECG is continuously recorded. Typically, if Brugada changes are present, the test will become positive within 5-10 minutes of starting the infusion.
As Ajmaline is short-acting, cardiac monitoring is generally required for only 2 hours after the procedure. If the test is negative, you can eat and drink after 30 minutes; if positive, you can eat and drink after 60 minutes.
Interpretation
Like all medical tests, a positive Ajmaline Study may be a ‘false positive’. Or, in other words, having a positive Ajmaline Study does not make a diagnosis of Brugada Syndrome. However, in the right setting - typical symptoms of Brugada Syndrome, or a strong family history of Brugada Syndrome - a positive Ajmaline Study is much more likely to be true than not. For this reason the Ajmaline Study should only be performed when there is a very good reason for doing it!
Risks
As Ajmaline is an anti-arrhythmic drug with strong effect on the electrical activity of the heart, there is a small risk of developing a serious cardiac arrhythmia during the infusion. This is the reason for strict cardiac monitoring. Overall, serious arrhythmia is very uncommon. But if it occurs, all of the necessary medication and equipment is immediately available for rapid treatment.
After the Test
Discharge from hospital will be 2-3 hours after the test if the ECG has returned to normal, and you are feeling well.
An appointment is made to see your doctor.
If the test is ‘positive’, you will be given some precautions to reduce your risk from Brugada Syndrome to as low as possible. But in general, if Brugada only appears when you have an Ajmaline Study, and you have no concerning symptoms such as sudden fainting, the risk of a serious rhythm complication is much less than 1% per year.
Precautions in the setting of a positive Ajmaline study
- Avoid ‘Brugada’ medications predicted to increase the risk of serious arrhythmia - a list may be found on www.brugadadrugs.org Check all medications either prescribed, or over-the-counter, against this list.
- Treat fever quickly. High body temperature may bring out the ECG changes of Brugada and increase the risk of serious arrhythmia. If you have fever: take paracetamol or ibuprofen and repeat every 4-6 hours aiming for a body temperature < 38C. If the temperature remains high, attend hospital for monitoring and treatment.
- Avoid heavy alcohol intake, particularly with a large meal. How much is too much? As a conservative measure, keep your intake below 3 standard drinks in any one sitting. Cocaine and other illicit drugs are also high risk.
- Inform your doctor if you:
- faint (syncope), especially with little warning, as this is an indicator of high risk
- have a ‘seizure’, as a faint may be misdiagnosed as a seizure
- wake with confusion in the night, have unexpected bed-wetting, or your partner notices strained, heavy breathing in the night - as these may be a sign of a faint/syncope while you sleep