Brugada Syndrome
Brugada Syndrome is an electrical disorder of the heart which may cause fainting (also called syncope) or, in rare cases, cardiac arrest. However, the majority of patients with Brugada Syndrome have no symptoms.
Diagnosis
Brugada Syndrome is diagnosed on the 12 lead ECG, usually in the context of symptoms or a typical family history. Sometimes the ECG changes of Brugada are discovered incidentally when an ECG is performed for another reason unrelated to the condition e.g. chest pain.
The ECG may show a typical ‘Type I’ pattern of Brugada (left) or a ‘Type II’ pattern (right). Type II is not diagnostic of Brugada Syndrome but makes it more likely that a Type I pattern will appear in future, either spontaneously or with drug provocation or fever.
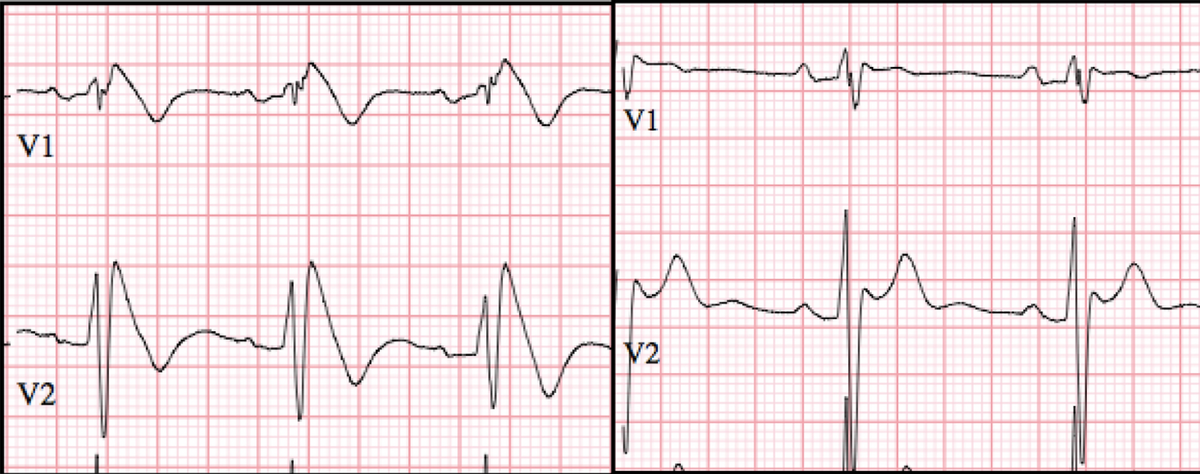
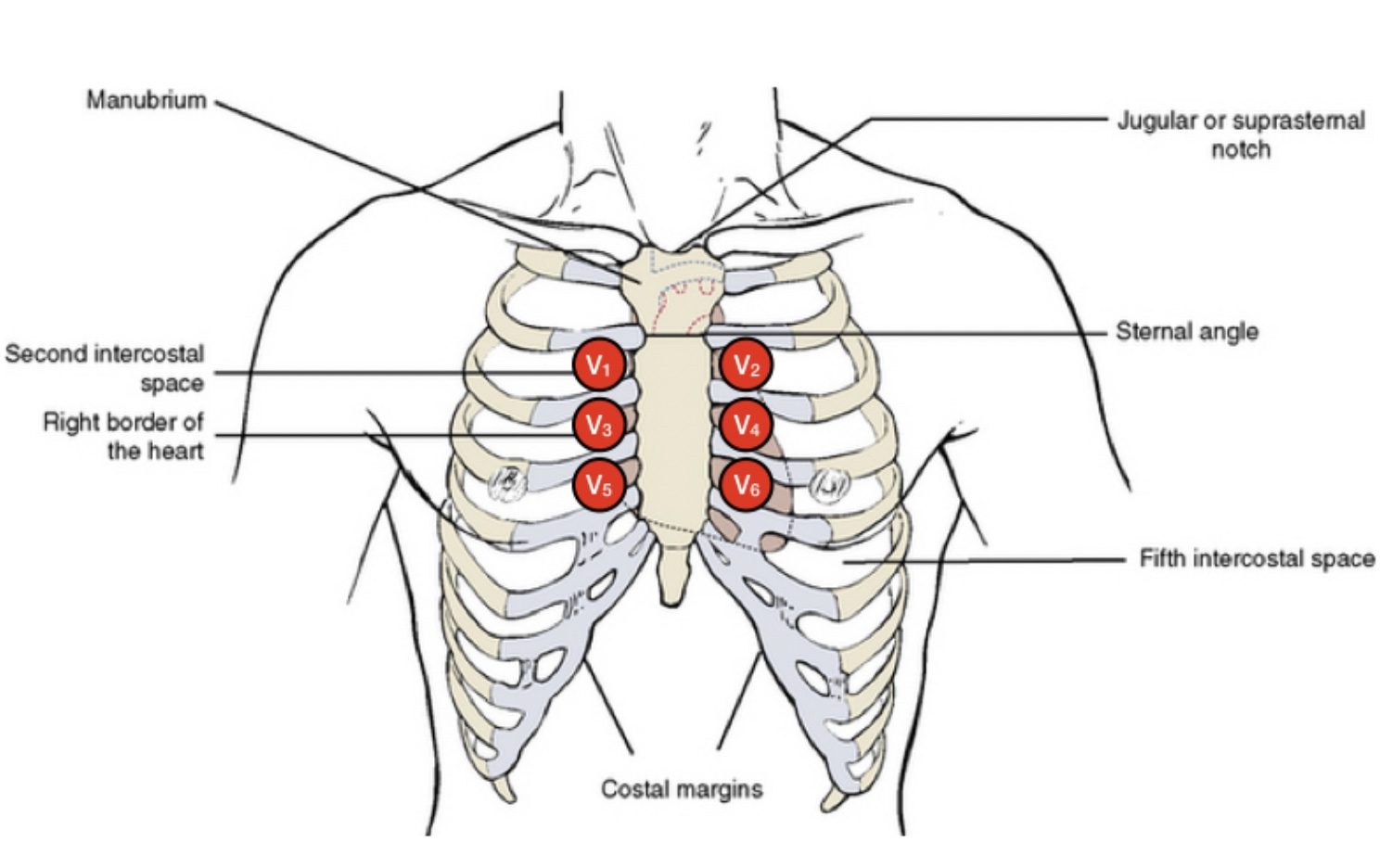
A standard ECG may miss the typical changes of Brugada which will only appear when the ECG ‘dots’ are moved to a higher location on the chest. As the ECG changes of Brugada come and go, a ‘provocation study’ using medication (either ajmaline or flecainide) is sometimes used to bring out the typical ECG changes.

The doctor may refer to your Brugada as (1) ‘spontaneous’ - that is, it appears in the absence of fever or a ‘provocation study’. (2) ‘fever induced’ - appearing in the context of fever or (3) ‘provoked’ - appearing when a drug like ajmaline or flecainide is given.
Inheritance
Brugada Syndrome is a genetic (inherited) disorder, but a single gene cause is identified in only 20% of individuals. The most common causative gene is called SCN5A and encodes a protein in the heart which is important for normal electrical conduction. If you have a variation in SCN5A as the cause of your Brugada Syndrome then there is a 50% chance that the abnormal gene will be passed down to each of your children.
In the remainder of individuals with inherited Brugada, it is likely that a collection of small changes in multiple different genes can ‘add up’ to the ECG changes of Brugada Syndrome. In this case the inheritance of Brugada Syndrome is more complex. While the chance of another member of your family having Brugada is increased, the risk is much less than 50%.
Treatment
Whether the Brugada ECG pattern appears spontaneously on the ECG, or else as a result of ajmaline or flecainide provocation, there are certain precautions advised to reduce the risk of arrhythmia:
- Avoid ‘Brugada’ medications predicted to increase the risk of serious arrhythmia - a list may be found on www.brugadadrugs.org Check all medications either prescribed, or over-the-counter, against this list.
- Treat fever quickly. High body temperature may bring out the ECG changes of Brugada and increase the risk of serious arrhythmia. If you have fever: take paracetamol or ibuprofen and repeat every 4-6 hours aiming for a body temperature < 38C. If the temperature remains high, attend hospital for monitoring and treatment.
- Avoid heavy alcohol intake, particularly with a large meal. How much is too much? As a conservative measure, keep your intake below 3 standard drinks in any one sitting. Cocaine and other illicit drugs are also high risk.
- Inform your doctor if you:
- faint (syncope), especially with little warning, as this is an indicator of high risk
- have a ‘seizure’, as a faint may be misdiagnoses as a seizure
- wake with confusion in the night, have unexpected bed-wetting, or your partner notices strained, heavy breathing in the night - as these may be a sign of a faint/syncope while you sleep
Risk Assessment
The risk of a life-threatening arrhythmia is highest in indivudals who have survivied a cardiac arrest, or who have a fainting episode due to an arrhythmia. In both cases, an implantable defibrillator is recommended.
Most faints (syncope) in patients with Brugada are due to benign causes - e.g. low blood pressure but it is important that you inform your doctor if you do faint as it is difficult to tell the difference between benign and dangerous fainting.
If you have Brugada ECG changes which occur spontaneously but have no symptoms, the risk of cardiac arrest is a little less than 1% per year, ~ 7% over 10 years. Some doctors recommend a drug called quinidine in this case but strong evidence in favour of its use is lacking.
If you do not have spontaneous ECG changes of Brugada, for instance if your ECG is only abnormal when you are given a drug like ajmaline or flecainide, then the risk of cardiac arrest over 10 years is ~ 2%. In this case we would only recommend the conservative measures explained above.
Historically, electrophysiology studies, or the presence of other ECG markers (such as fragmentation, or early repolarisation), have been used to refine the risk of arrhythmia in an individual. The use of these markers/tests can be discussed with your physician.
Genetic Referral
If you have Brugada Syndrome, or are treating an individual with Brugada Syndrome, then a referral may be made to the Cardiac Genetic Clinic at Royal Melbourne Hospital c/o Dr Mark Perrin and Ms Tina Thompson (Clinical Nurse Consultant), to discuss the utility of genetic testing.
Dr Mark Perrin c/o Tina Thompson | Clinical Nurse Consultant Genomic Medicine | Level 2, Centre Block Royal Melbourne Hospital | Grattan Street, Parkville VIC 3050 T: +61 3 9342 7151 | F: +61 3 9342 4267