Atrial Fibrillation Ablation
Atrial fibrillation is a rapid and irregular heartbeat which may lead to blood clots, stroke, and heart failure. It is often felt as an irregular palpitation, shortness of breath, and fatigue.
Catheter ablation is a common procedure used to control symptomatic atrial fibrillation when medication is not effective, not tolerated due to side effects, or as a patient preference over daily medication.
What is Catheter Ablation of Atrial Fibrillation?
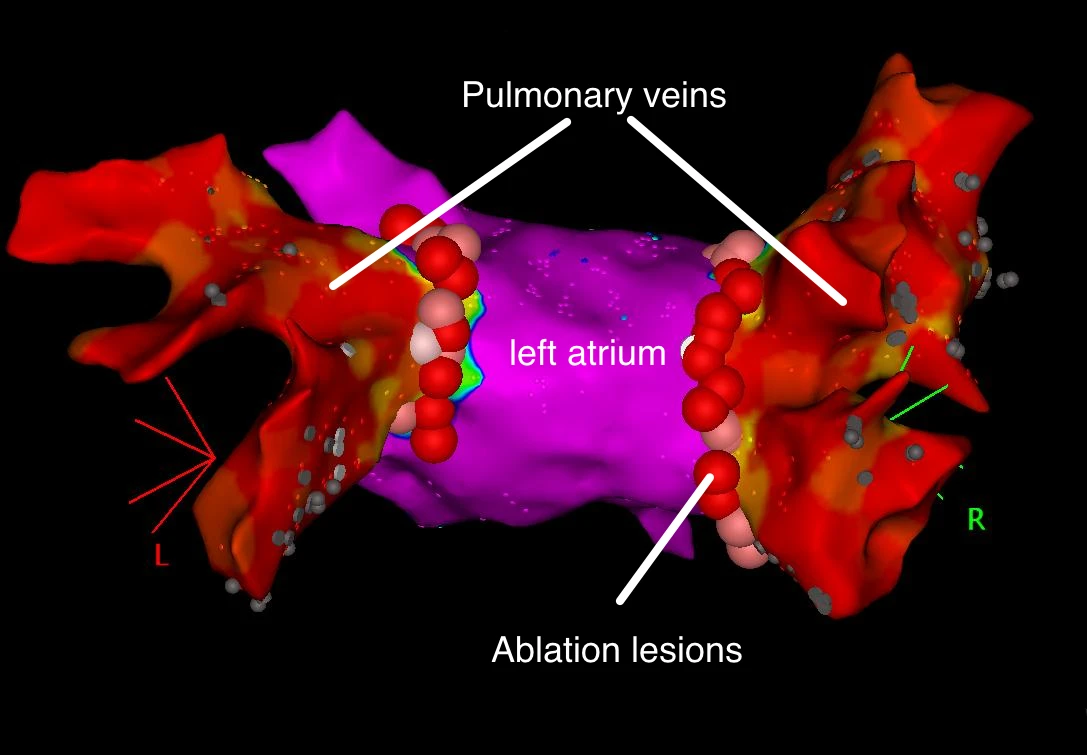
Catheter ablation of atrial fibrillation is also called ‘Pulmonary Vein Isolation’. The heart receives oxygen-rich blood from the lungs through large blood vessels known as the pulmonary veins. These veins can sometimes ‘fire’ off extra heartbeats which trigger atrial fibrillation. Catheter ablation isolates the pulmonary veins from the heart. They still carry blood as they should, but can no longer trigger atrial fibrillation.
Radiofrequency Pulmonary Vein Isolation
What Happens During the Procedure?
If you are not already taking an anti-coagulant (such as rivaroxaban, apixaban or dabigatran) this will be commenced a few weeks prior to the ablation and will continue for at least 3 months following the procedure. In some cases, it will be recommended that the anti-coagulant continue indefinitely.
Catheter ablation is performed in hospital. The procedure starts with a general anaesthetic. When you are asleep, a trans-oesphageal echocardiogram (TOE) is performed, this is a small tube with an ultrasound probe which is placed in the oesophagus, and directed at the heart to check that there is no blood clot within the left atrium.
Catheters, which are thin wires, are then advanced through a small incision in the femoral vein (a large vein at the top of the leg).
The catheters are advanced carefully to the heart. The main goal of this procedure is to prevent abnormal electrical signals exiting from the pulmonary veins. Hence, the catheter is used to deliver energy (either pulse field energy (PFA), radiofrequency ‘burning’ or cryoablation ‘freezing’) to create scar around the pulmonary veins which electrically isolates the vein from the heart.
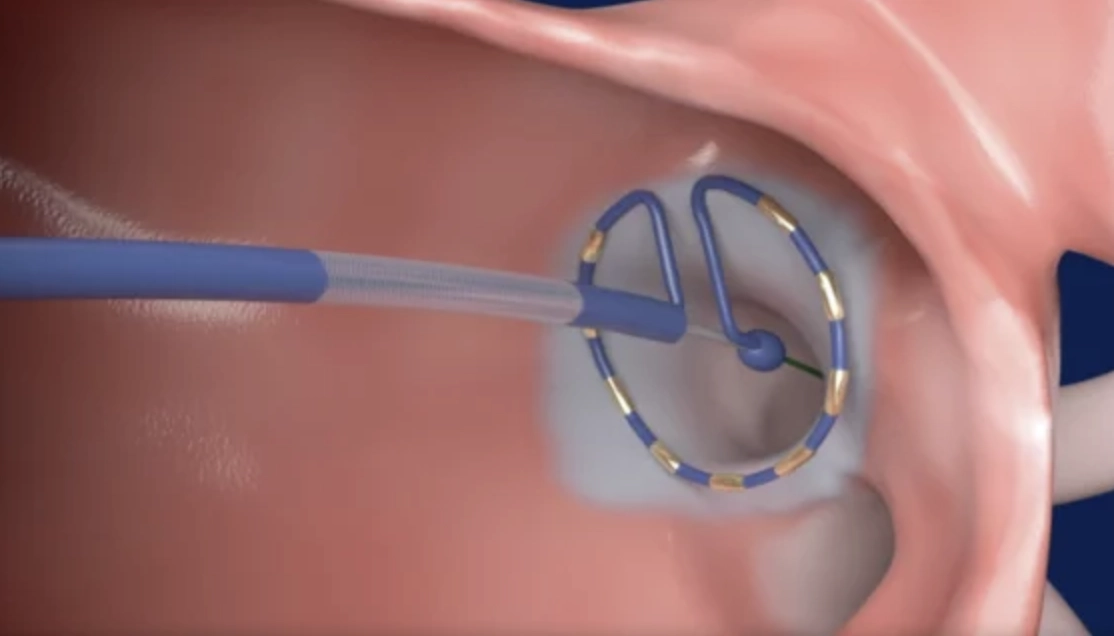
Pulse Field Ablation using the PulseSelect System
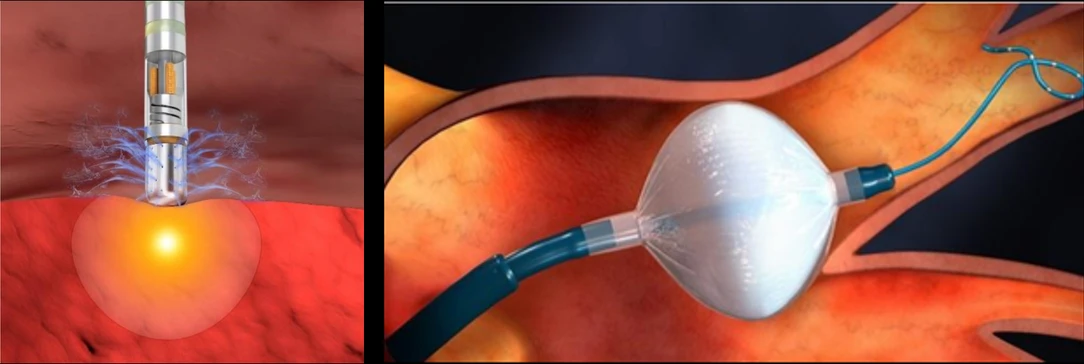
Radiofrequency Catheter on Left and Cryoballoon Catheter on Right
In some cases, the ablation catheter is also used to treat other areas of the atria, away from the pulmonary veins, which are triggering atrial fibrillation.
The procedure typically takes between 1 and 2.5 hours.
After pulmonary vein isolation is confirmed, all of the catheters are removed from the body. A stitch is placed to prevent bleeding from the femoral vein; this is removed later on.
You remain in hospital overnight and, if all is well, will go home in the morning.
Follow Up
Common Symptoms Following Catheter Ablation
It is normal to feel some fatigue, and mild shortness of breath in the days to weeks after the procedure. Some mild chest pain is also common - generally when you take a deep breath - which will clear over a few days.
As you will be on anti-coagulant medication, and given extra ‘blood thinning’ during the procedure, you will have some bruising in the leg where the catheters are introduced. This may look quite impressive but will clear over 3-4 weeks.
Lastly, you may have some atrial fibrillation in the 2-3 weeks after ablation. This is often due to inflammation from the procedure itself, and does not necessarily mean that the procedure has not worked. If it is inflammation then it will go away within weeks.
Symptoms That Need Attention
It is not normal to experience:
- severe pain in the chest
- fever
- any neurological symptoms (such as weakness, loss of vision, or difficulty speaking)
- increasing swelling at the femoral vein (but a small grape size firmness is normal)
- faint
If you have any of these symptoms you should go to emergency for review and have them contact Dr Perrin.
Follow Up Appointment
You will be seen 6-8 weeks following the procedure for general review and to arrange ongoing follow-up.
If atrial fibrillation returns, the procedure is performed a second time, most often as a ’touch up’ of the original ablation to re-isolate the pulmonary veins. About 1 in 4-5 people require a second ablation.
Success
Catheter ablation works best when atrial fibrillation comes and goes - we call this ‘paroxysmal AF’. In this case, atrial fibrillation may be supressed in up to 70-80%.
When atrial fibrillation is present all the time, also called ‘persistent AF’, the success rate is less. Control of atrial fibrillation, that is - being in normal rhythm the vast majority of the time - is achieved in 50% and more often requires multiple procedures to achieve this outcome.
Risks
The risks of atrial fibrillation ablation include:
2% risk of bleeding at the femoral puncture site occasionally requiring vascular surgery to fix, pericardial effusion (fluid around the heart which requires drainage), reaction to the anaesthetic
0.2% risk of a disabling complication including: stroke, heart attack, phrenic nerve palsy (which may cause ongoing shortness of breath), stenosis (narrowing) of the pulmonary veins requiring treatment, emergency surgery.
[Of note, the newer technology of “Pulse Field Ablation” (PFA) carries no risk of permanent phrenic nerve palsy, or pulmonary stenosis]
0.05% risk of death.
Summary
Catheter ablation is an effective procedure to control the symptoms and burden of atrial fibrillation, particularly when medication is ineffective or intolerable.