Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT) is a genetic condition where the heart develops dangerous rhythms (polymorphic ventricular tachycardia), especially during emotional stress or exercise.
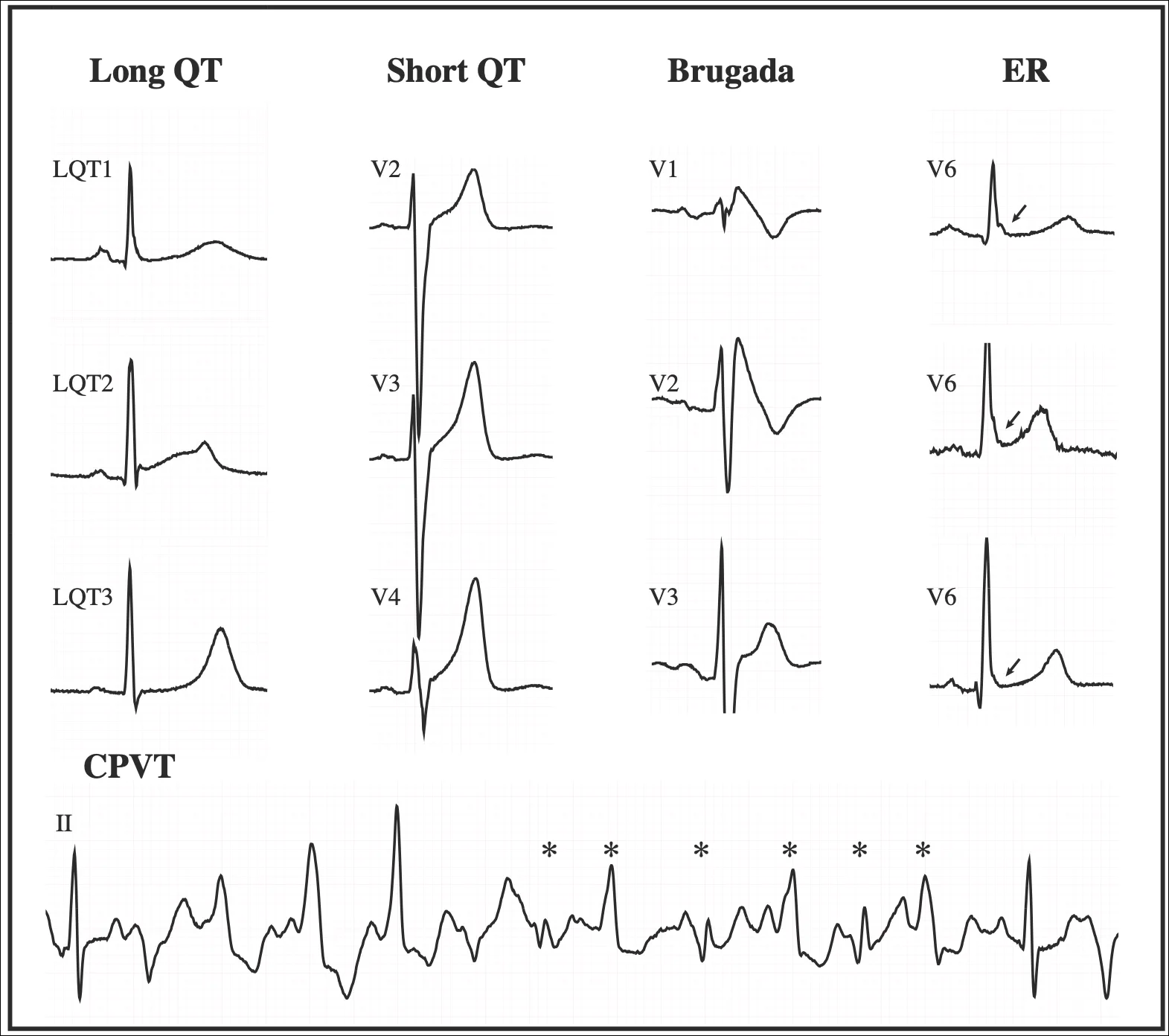
Cardiac Genetic Conditions
How Does it Present?
People with CPVT often faint during childhood or adolescence. It’s essential to diagnose CPVT early because it can be potentially fatal if untreated.
Symptoms of fainting or ‘seizure’ usually start between 7 and 10 years of age but can appear later, especially in women and those without a known genetic cause.
Other conditions, like the Long QT syndrome, have similar symptoms but may occur at different times or in response to different triggers.
Diagnosis
The condition is suspected when syncope (fainting) occurs in response to exercise (e.g. swimming, or running), especially when there is a family history sudden cardiac death.
The ECG might look normal in someone with CPVT. So to make the diagnosis, the heart needs to be put under stress.
The main way to diagnose CPVT is an exercise test (treadmill test with a ‘sprint’ protcol), where the heart rhythm is monitored during physical activity. Close to 100% of CPVT patients show heart rhythm problems during this test.
Other tests like adrenaline infusions and long-term heart monitors can be useful in some situations.
Genetic Testing
Primary Genes Involved:
RYR2: This gene encodes for the cardiac ryanodine receptor. Mutations here are the most common cause of CPVT. CSQ2: This gene is responsible for producing calsequestrin-2. Mutations in CSQ2 are another cause of CPVT, but they are less common than RYR2 mutations. Usually, you need two ‘bad’ CSQ2 genes to develop the condition; uncommonly, one ‘bad’ CSQ2 is enough.
Possible Genetic Testing Results:
- Positive (Pathogenic Variant Found): A mutation is found in either the RYR2 or CSQ2 gene that is known to cause CPVT.
- Negative (No Pathogenic Variant Found): No mutations linked to CPVT are found in the tested genes. It doesn’t entirely rule out CPVT, as not all genetic mutations are known or tested.
- Variant of Uncertain Significance (VUS): A change is found in the gene, but it’s unclear if this change causes CPVT or is harmless.
Conditions that Look Like CPVT
There are other genetic conditions, like KCNJ2 disease (Andersen Tawil Syndrome), that have similar symptoms to CPVT; long QT syndrome may also present with fainting. If a patient’s family has a mix of symptoms that don’t match CPVT perfectly, genetic testing for these other conditions might be necessary.
Similarly, rapid chaotic heart beating (called polymorphic ventricular tachycardia) may occur when the heart is structurally abnormal e.g. coronary artery disease, valve dysfunction, previous myocarditis, or cardiomyopathy. However, in CPVT the heart is almost always normal. So it is important to rule out these other conditions before making a diagnosis of CPVT.
Treatment
-
Exercise Restriction is recommended in most cases, particularly avoiding high-intensity activity. When medication is effective most patients may return to moderate intensity exercise.
-
Medication
- Beta blockers, specifically the long acting agent Nadolol is recommended for all patients with CPVT. It is typically started at 40mg a day and increased to 80-120mg a day depending on response.
- Flecainide is used if nadolol alone fails to suppress the abnormal heart rhythm. It is started in addition to Nadolol, usually at 50mg twice a day increasing up to 100-150mg twice a day.
- Left Cardiac Sympathetic Dennervation is a surgical procedure where certain nerves (the sympathetic chain) on the left side of your chest, which send signals to your heart, are removed. By cutting or blocking these nerves, the heart rhythm may be less sensitive to exercise or emotional induced arrhythmia. This is an invasive procedure with small risk of infection and nerve related pain; in the long term, your left arm will be cooler and drier than the other side. Rarely (1%), a condition called Horner’s syndrome (drooping of the eyelid which is generally mild) may develop; similarly rare, facial ‘redness’ may develop on one side. For these reasons, it will generally be reserved for where medication is ineffective or not tolerated.
- Implantable Cardiac Defibrillator (ICD or defibrillator) is a device which can deliver a shock to the heart in the event of a dangerous heart rhythm. This is reserved for patients with symptoms despite medication or LCSD, or who are deemed to be at a particularly high risk of a life-threatening event. It should never be the only treatment but is employed as a ‘backup’ measure in patients on the medication detailed above.
Prognosis
If treated, there is no reason why a patient with CPVT cannot live a long and enjoyable life. Most of the danger of this condition comes when the diagnosis is missed, or not known.