Implantable Defibrillator (ICD)
Implantable Defibrillator (ICD)
An implantable cardioverter defibrillator (ICD) is a device for individuals who are at risk of a life-threatening heart rhythm disorder called ‘ventricular arrhythmia’. It recognises abnormal heart rhythms and either ‘paces’ the heart out of the bad rhythm, or delivers an electric shock to restore normal rhythm.
Indications
- Previous cardiac arrest due to a ventricular arrhythmia
- Certain inherited heart conditions that predispose to ventricular arrhythmia
- Specific heart muscle conditions such as dilated cardiomyopathy (DCM), ischaemic cardiomyopathy, hypertrophic cardiomyopathy, or arrhythmogenic cardiomyopathy (AC) which predispose to ventricular arrhythmia
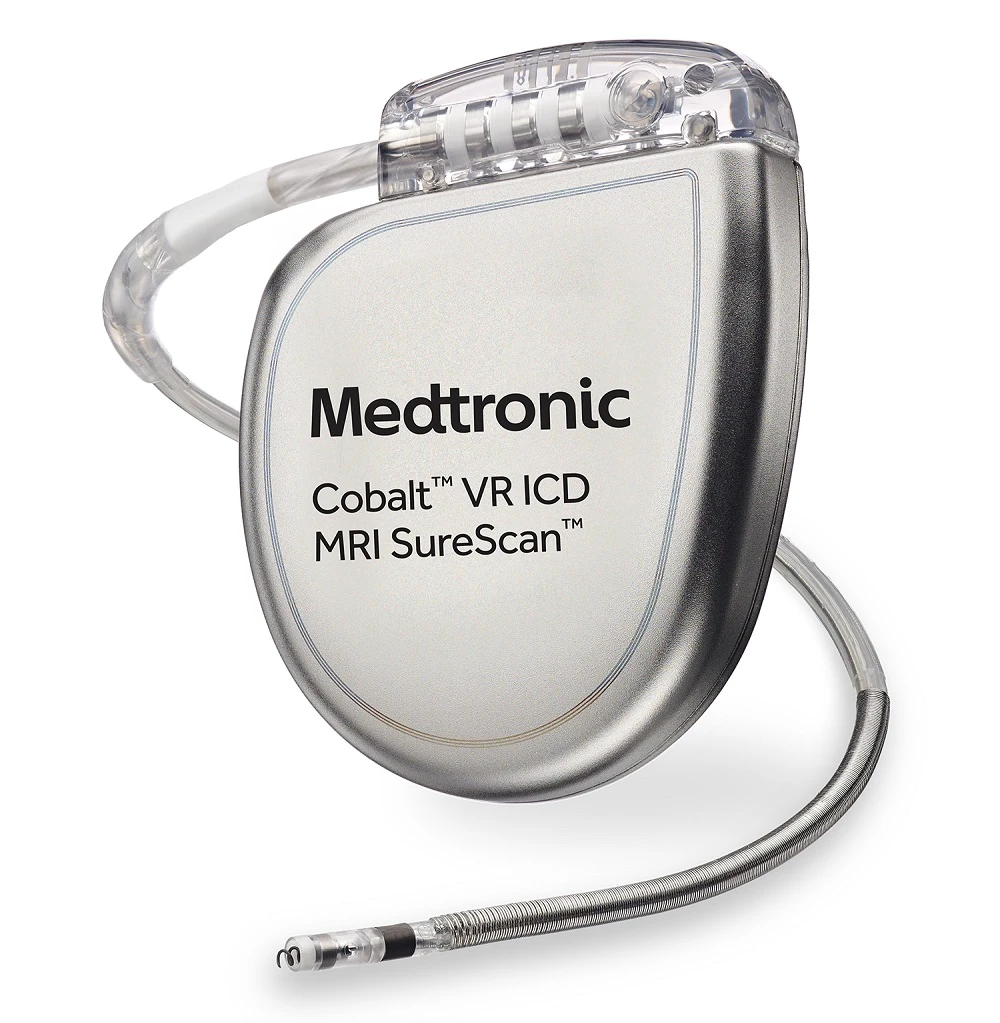
Single lead defibrillator
Implantation
A defibrillator is made up of a generator (about 4-5cm long, and 12mm thick), and one or more leads. Each lead is a thin wire that runs from the generator to the heart.
A defibrillator has the same function as a pacemaker, but with the added ability to shock the heart in the event of arrhythmia.
The procedure is performed in hospital under sedation or with general anaesthesia. After antibiotic medication is given to help prevent infection, a small incision is made below the collar bone. A ‘pocket’ is then made under the skin to house the generator. One or 2 leads are passed into the nearby vein - called the subclavian vein - and then into the heart where they are attached to the inner lining of the heart by small screws. Finally, the wound is closed with absorbable sutures and a dressing placed over the incision.
Once the defibrillator is implanted it is programmed to suit the specific needs of the individual. This can include setting the rate at which the device sends impulses to the heart, and the specific abnormal rhythms which it will treat.
Risks
While an ICD implantation is a relatively safe procedure, there are potential risks as with any surgical intervention.
1% risk of lead dislodgement, pneumothorax (air around the lung), pericardial effusion (blood around the heart requiring drainage), and infection.
There are also small risks of mechanical malfunction of the device or lead which may require surgical revision of the device. There is a small ongoing risk of receiving a shock from the device that is not needed - ‘inappropriate shock’ - due to device malfunction or misinterpretation of an abnormal heart rhythm.
Lastly, as the defibrillator lead passes through the tricuspid valve which separates the right atrium from the right ventricle, the valve may become leaky. This is usually mild and does not cause symptoms, but occasionally may be significant.
The risk of a very serious complication including stroke, emergency surgery, or heart attack is 1:1000 or less.
Post-Procedure Care
You will remain in hospital overnight after the procedure. A CXRAY is performed in the evening to check the positioning of the device and the lead. In the morning, a final check of the device is made before discharge home.
Your GP will remove the wound dressing 5-7 days after the procedure, and you will be seen 4 weeks later either by Dr Perrin, or in the device clinic at University Hospital Geelong.
On discharge from the hospital a remote monitor is given which monitors the defibrillator function when at home. In some cases (depending on the particular device), an iPhone or Android application may be used to monitor the defibrillator.