Idiopathic Ventricular Fibrillation
When a ventricular fibrillation cardiac arrest occurs, the cause is usually clear. Severe illness, coronary artery disease, and cardiomyopathy, are all common. But in some rare cases it is not. Ventricular fibrillation may occur when a person is well, and in a heart that appears to be normal. In this case the cause is termed ‘idiopathic’, medical-speak for ‘we do not know’.
Idiopathic ventricular fibrillation (IVF) can be defined in several ways. In strict terms it is ventricular fibrillation where all other causes have been excluded. However, in a real-world scenario, this definition may expand to include cases where cardiac testing is incomplete, and genetic testing has not been performed.
Mechanism
Ventricular fibrillation (VF) is either triggered by a premature ventricular contraction (PVC), or more commonly by degeneration of ventricular tachycardia (VT) into ventricular fibrillation.
Ventricular tachycardia (VT) usually occurs in the setting of structural heart disease. In this scenario, scar within the heart predisposes to rapid heart beating (VT) which degenerates into VF.
Idiopathic ventricular fibrillation (IVF) is usually triggered by a PVC, which is short-coupled to the previous beat.
In fact, short-coupled PVC triggered IVF, is a well described condition with a typical onset, and common therapy (quinidine). When IVF is recurrent, short-coupled PVCs arising in the Purkinje system are almost always the mechanism.
Diagnostic Procedures for Idiopathic VF
There is no diagnostic procedure for this condition. Instead, the diagnosis comes from ruling out alternative causes; and is supported, in some cases, by the recording of a typical ECG.
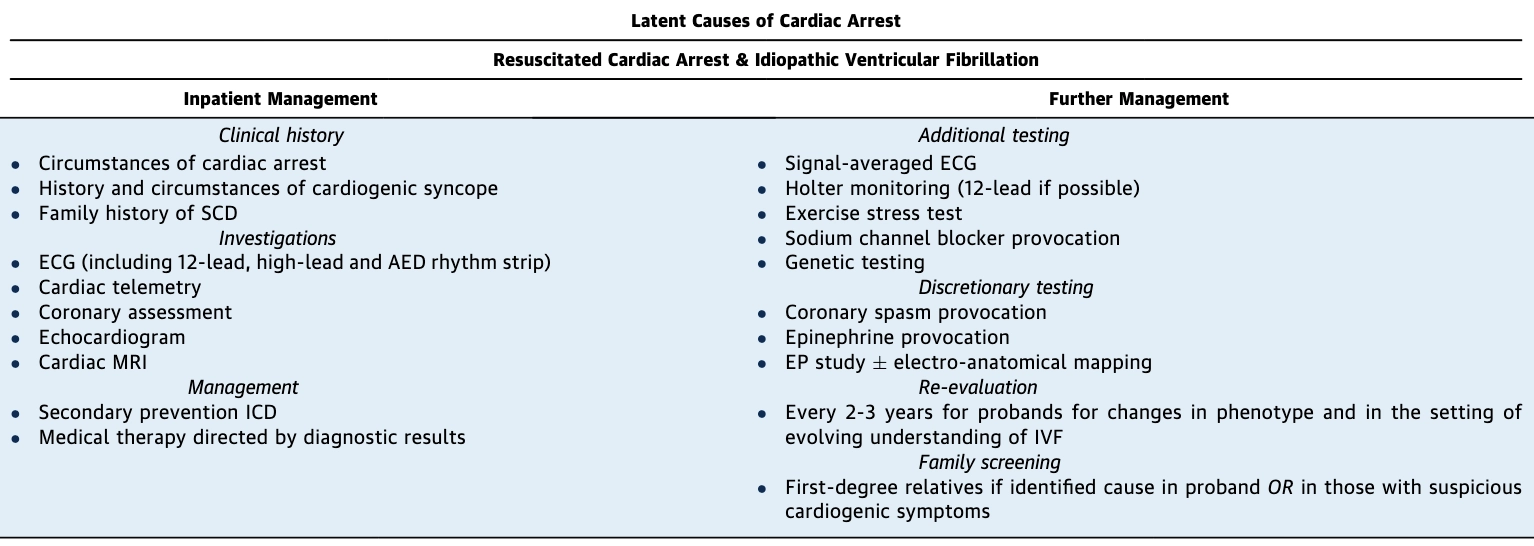
Investigation and Treatment for IVF. From: Krahn AD et al. Latent Causes of Sudden Cardiac Arrest. JACC EP 2022
Short-Coupled PVC ‘Idiopathic’ VF
Electrophysiological examination of IVF identifies subtle structural abnormality in some (usually in the RV, occasionally in LV or both ventricles), and Purkinje PVCs in others, with both present in some.
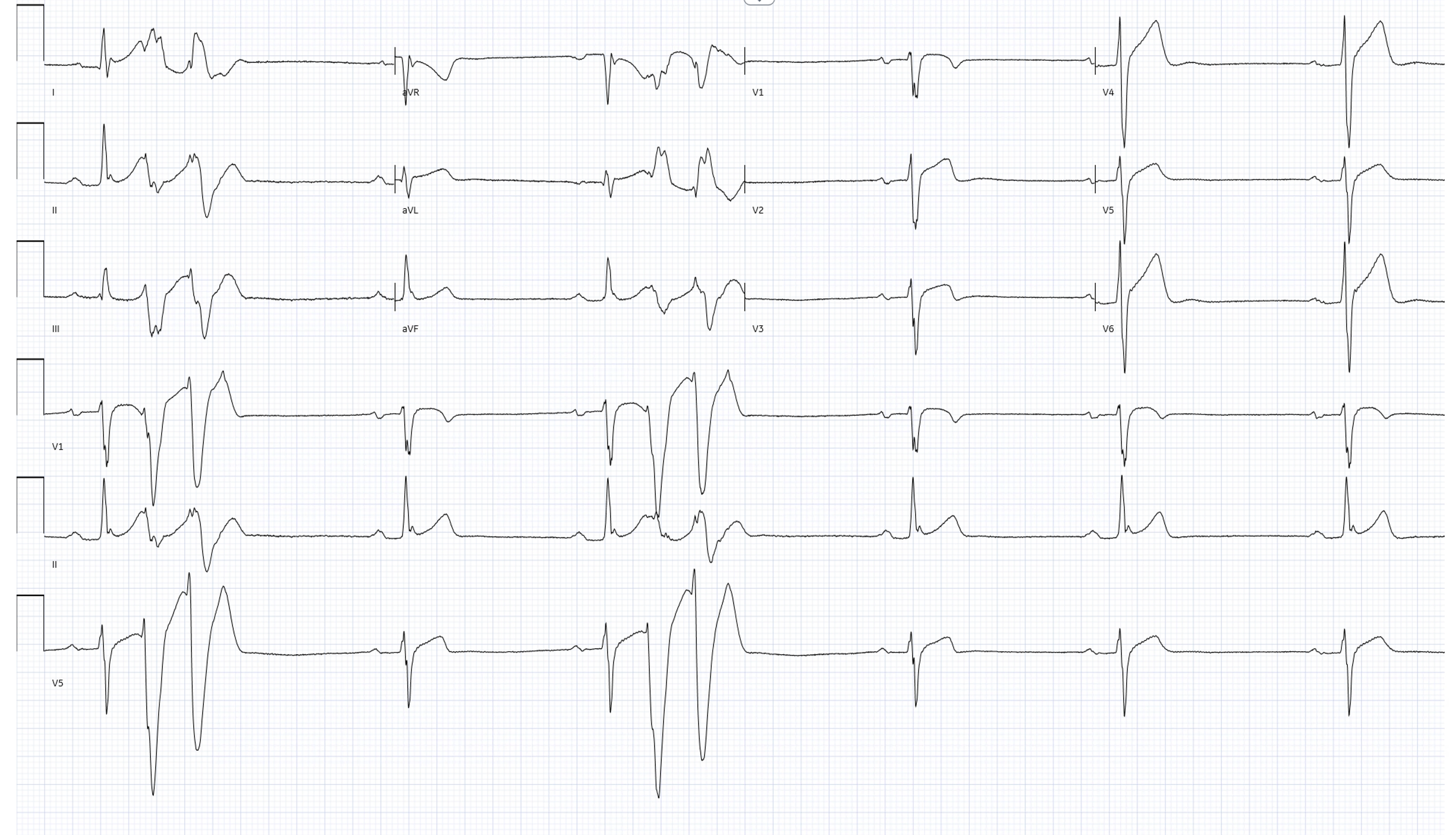
Typical Short-Coupled PVC of IVF
Genetics
The more thorough the work-up of IVF, the less likely a genetic cause will be found. Overall the genetic yield is 2-12%, and mostly identifies abnormalities in cardiomyopathy or arrhythmia genes, suggesting a concealed structural or electrical substrate, at least at the resolution of our current diagnostic testing.
When the mechanism of VF is short-coupled PVCs, genetic abnormalities in CALM1, IRX3, RYR2, or the promoter haplotype in DPP6 (predominantly Dutch heritage) are possible.
Equally, if thorough testing is performed on an individual with ventricular fibrillation and fails to find a cause; and genetic testing is negative in that individual; then it is unlikely that screening will identify an abnormality in family members.
Treatment
After cardiac arrest, or syncope due to IVF, a defibrillator will be placed.
If VF is recurrent, quinidine is the most effective medication. Then, if this is not working or not tolerated, consideration is given to catheter ablation of the triggering PVC or underlying substrate.
Summary
The condition Idiopathic VF, when other causes are properly excluded, is most commonly due to short-coupled PVCs from Purkinje cells, often in the setting of subtle structural abnormalities in the RV and LV. The remaining cases remain properly idiopathic, or are an electrical manifestation of a concealed cardiomyopathy or arrhythmia syndrome (perhaps 2-10% overall) below the diagnostic resolution of current cardiac testing to identify. An ICD is protective, and quinidine will often suppress recurrent episodes.