Wolff Parkinson White
Wolff Parkinson White
Wolff Parkinson White (WPW) syndrome, is a heart condition where there is an extra (“accessory”) electrical pathway in the heart, leading to episodes of rapid heart rate.
What is an Accessory Pathway?
Normal electrical activity of the heart passes from the sinus node in the right atrium, through the AV node (in the middle of the heart) and into the ventricles. There should be one connection which joins the atria and the ventricles.
Some people are born with an extra (accessory) pathway. So they have two or more pathways from the back to the front of the heart.
This accessory pathway often gives the standard ECG an unusual appearance with an initial slurring of the ventricular activation which is known as a ‘delta wave’. If you have a ‘delta wave’ you have Wolff Parkinson White.
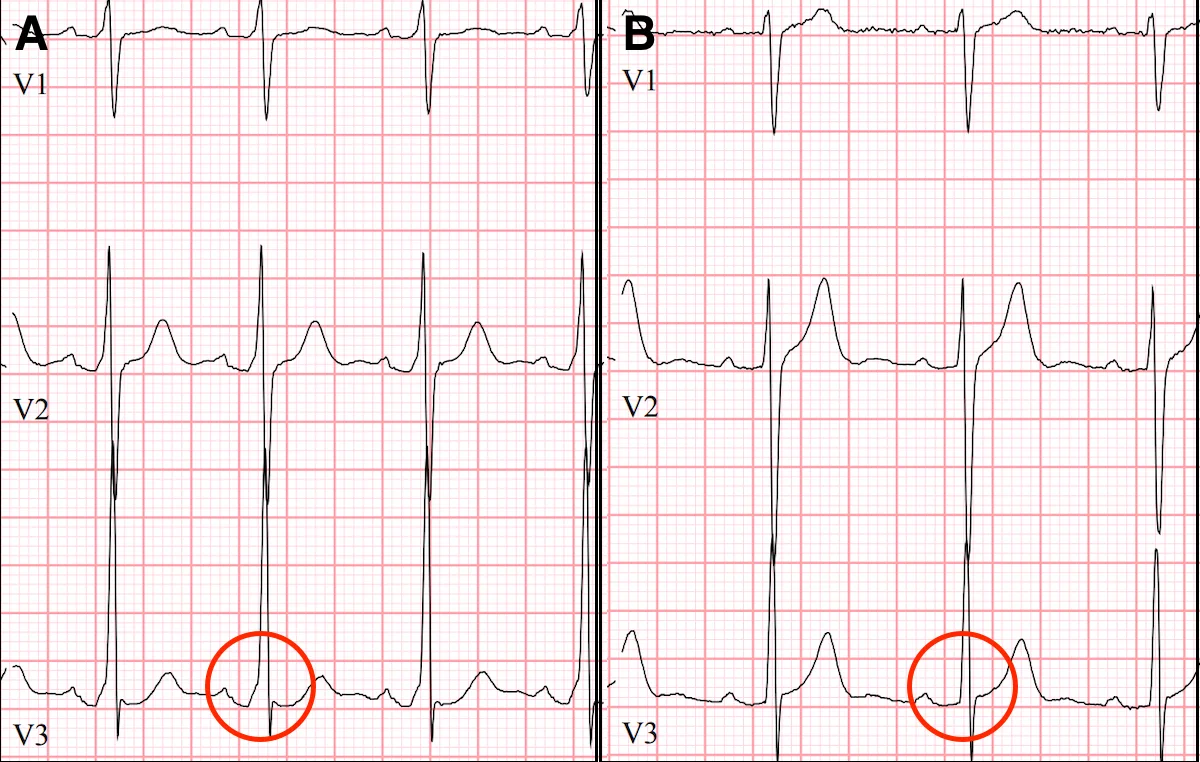
ECGs of WPW Before (left) and After (right) Catheter Ablation. In the left panel a slurring is seen called a 'delta wave'. After ablation (right) the 'delta wave' is gone
In some cases, an accessory pathway is present but there is no ‘delta wave’. We call this a concealed accessory pathway. It is diagnosed by an electrophysiology study.
Symptoms
Some cases of WPW are picked up on an ECG which is performed for other reasons. That is, it is an incidental finding. In many cases the accessory pathway causes no symptoms.
In others, the diagnosis is made after typical symptoms: most commonly the sudden onset of a racing heart; less commonly with a fainting episode, and only very rarely with more serious arrhythmia causing a cardiac arrest.
Is it Dangerous?
In the vast majority of cases WPW does not cause dangerous arrhythmia. However, the symptoms of the condition may be very troubling.
In rare cases, WPW may predispose to a condition called atrial fibrillation. This arrhythmia is potentially dangerous in the setting of WPW because the extra pathway allows the ventricles at the front of the heart to beat very quickly. This may cause a cardiac arrest.
Markers of High Risk There are certain features that increase this serious risk of WPW:
- supraventricular tachycardia (SVT)
- male sex
- WPW diagnosed before age 20
- history of atrial fibrillation
- competitive athletics or high-intensity exercise
- structural heart disease (either thickening or weakening of the heart)
If one or more of these features are present, then we may consider performing an electrophysiology study. At this study, which is performed in hospital, the extra pathway (if high risk) can be ablated thus eliminating the risk.
In other cases of WPW, especially when asymptomatic, an exercise test may be enough to rule out a high risk accessory pathway.
How Common is this Condition?
WPW is seen in about 0.2% of the population, and of this group many will have no symptoms at all.
Occasionally, WPW may be part of a cardiac syndrome: either genetic thickening of the heart, also called hypertrophy; or as part of a condition called Ebstein’s anomaly where the tricuspid valve on the right side of the heart is displaced.
But more commonly, WPW occurs alone in the setting of a structurally normal and healthy heart.
Treatment
If the accessory pathway is considered to be low risk, and you have no symptoms, then no treatment is required.
If you have troublesome symptoms, or documented arrhythmia (such as SVT), then an electrophysiology study is performed with catheter ablation.
Catheter Ablation
In this procedure, thin flexible wires called catheters are advanced carefully to the heart under Xray or 3D guidance. The catheter is placed over the pathway and used to deliver radiofrequency energy. This heats the tissue and ‘scars’ the pathway thus eliminating its conduction. The success rate is around 80-90% on the first procedure. In some cases the pathway may recover and the procedure needs to be performed a second time. In other cases, the risk of treating the pathway is considered too high - this is particularly the case when the extra pathway lies very close to the normal AV node, and where treatment of the abnormal tissue may damage normal tissue placing you at a higher risk of needing a lifelong pacemaker.
Risks of the procedure include:
- bleeding/bruising/pseudoaneurysm at femoral vein in leg where catheters are introduced
- bleeding around the heart (pericardial effusion) requiring drainage (<1%)
- need for a pacemaker (<1%)
- the risk of more serious complications including stroke, heart attack, or emergency surgery to correct a serious complication, is 0.1%
Summary
WPW is a common cause of supraventricular tachycardia (racing heart), especially in younger individuals.
It is generally benign but the symptoms can be distressing.
In rare cases it may predispose to more serious rhythm abnormalities and cause a cardiac arrest.
If you have symptoms due to WPW, or other features of a high-risk pathway, then catheter ablation to eliminate the pathway is recommended. This is a curative procedure. If follow-up ECGs are normal, and you have no symptoms, then you will not need to worry about this condition ever again.